by Chris Durst Jan. 10, 2023
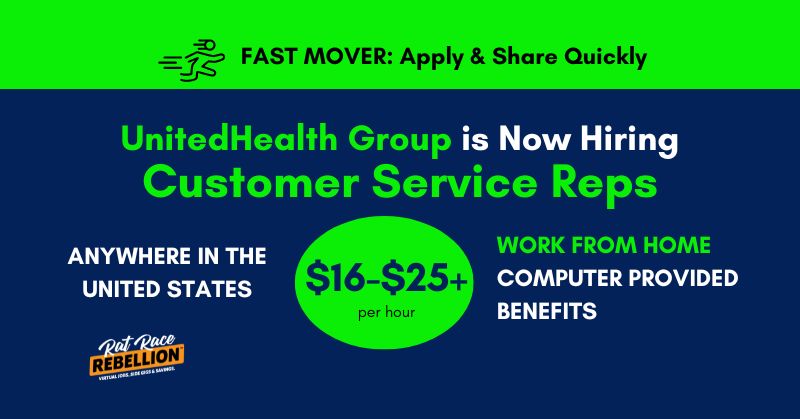
UnitedHealth always has a large number of work at home jobs available. But their Customer Service jobs are rare and very popular. So you should apply or share quickly if you’re interested.
If you have a “helpful personality” and are ready to start a full-time work from home job with a larger company, this could be a fit.
They are hiring “from anywhere within the U.S.”
The company will provide a computer.
Applicants should have 1+ years customer service experience in an office or professional setting.
Pay is listed for several states and appears to be in the $16-$25+/hr. range.
“In addition to your salary, UnitedHealth Group offers benefits such as, a comprehensive benefits package, incentive and recognition programs, equity stock purchase and 401k contribution (all benefits are subject to eligibility requirements).”
Here’s what the company has to say about the openings:
You’ll enjoy the flexibility to telecommute* from anywhere within the U.S. as you take on some tough challenges.
Welcome to one of the toughest and most fulfilling ways to help people, including yourself. We offer the latest tools, most intensive training program in the industry and nearly limitless opportunities for advancement. Join us and start doing your life’s best work.SM
Even if you have no prior experience, we have training classes starting soon to help you build the successful career that you want – apply today! We provide the support and structure, you provide the interest and motivation.
You like working with people. Even more so, you like helping them. This is your chance to join a team dedicated to helping our members and their families every day. In this joint role as a Customer Service Representative, you’ll join us on a mission to not only deliver the best customer service in the health care industry, but the best customer service. Period. Your compassion and customer service expertise combined with our support, training and development will ensure your success. This is no small opportunity. This is where you can bring your compassion for others while doing your life’s best work.SM
In this role, you play a critical role in creating a quality experience for the callers that you connect with and those that you correspond with. Every interaction gives you that opportunity to improve the lives of our customers and exceed their expectations. You’ll spend the majority of your day by responding to calls from our members and help answer questions and resolve issues regarding health care eligibility, claims and payments. You’ll also spend a portion of your time reviewing, researching and processing healthcare claims with the goal to ensure that every claim has a fair and thorough review.
This position is full-time (40 hours/week) Monday to Friday. Employees are required to have flexibility to work any of our 8-hour shift schedules during our normal business hours of 08:30am – 05:00pm CST.
*All Telecommuters will be required to adhere to UnitedHealth Group’s Telecommuter Policy.
Primary Responsibilities:
- Answer incoming phone calls from customers and identify the type of assistance the customer needs (i.e. benefit and eligibility, billing and payments, authorizations for treatment and explanation of benefits (EOBs)
- Ask appropriate questions and listen actively to identify specific questions or issues while documenting required information in computer systems
- Own problem through to resolution on behalf of the customer in real time or through comprehensive and timely follow-up with the member
- Review and research incoming healthcare claims from members and providers (doctors, clinics, etc) by navigating multiple computer systems and platforms and verifies the data/information necessary for processing (e.g. pricing, prior authorizations, applicable benefits)
- Ensure that the proper benefits are applied to each claim by using the appropriate processes and procedures (e.g. claims processing policies and procedures, grievance procedures, state mandates, CMS/Medicare guidelines, benefit plan
documents/certificates) - Communicate and collaborate with members and providers to resolve issues, using clear, simple language to ensure understanding
- Meet the performance goals established for the position in the areas of: efficiency, accuracy, quality, member satisfaction and attendance
You’ll be rewarded and recognized for your performance in an environment that will challenge you and give you clear direction on what it takes to succeed in your role as well as provide development for other roles you may be interested in.
Required Qualifications:
- High school diploma / GED (or higher) OR 10+ years of equivalent work experience
- 1+ years customer service experience in an office or professional setting
- Successfully complete the training classes and demonstrate proficiency of the material
Telecommuting Requirements:
- Required to have a dedicated work area established that is separated from other living areas and provides information privacy
- Ability to keep all company sensitive documents secure (if applicable)
- Must live in a location that can receive a UnitedHealth Group approved high-speed internet connection or leverage an existing high-speed internet service
Preferred Qualifications:
- Familiarity with medical terminology, health plan documents, or benefit plan design
- Prior experience utilizing multiple systems/platforms while on a call with a member
Soft Skills:
- Demonstrated ability in using computer and Windows PC applications, which includes strong keyboard and navigation skills and learning new computer programs
- Demonstrated ability to quickly build rapport and respond to customers in a compassionate manner by identifying and exceeding customer expectations (responding in a respectful, timely manner, consistently meeting commitments)
- Demonstrated ability to listen skillfully, collect relevant information, determine immediate requests and identify the current and future needs of the member
- Flexibility to customize approach to meet all types of member communication styles and personalities
- Proficient problem-solving approach to quickly assess current state and formulate recommendations
- Proficient conflict management skills to include ability to resolve issues in a stressful situation and demonstrate personal resilience
- Ability to multi-task as well as the ability to understand multiple products and multiple levels of benefits within each product
- Ability to work regularly scheduled shifts within our hours of operation including the training period, where lunches and breaks are scheduled, with the flexibility to adjust daily schedule and work over-time as needed
CLICK HERE for full details and to apply. For more jobs like these, check our Newest Jobs & Gigs page. To be the first to hear about jobs like these, like our Facebook page and check your feed for our posts. May you be working from home soon!
PLEASE SHARE this post – turn your friends into Rat Race Rebels!
[social_warfare]